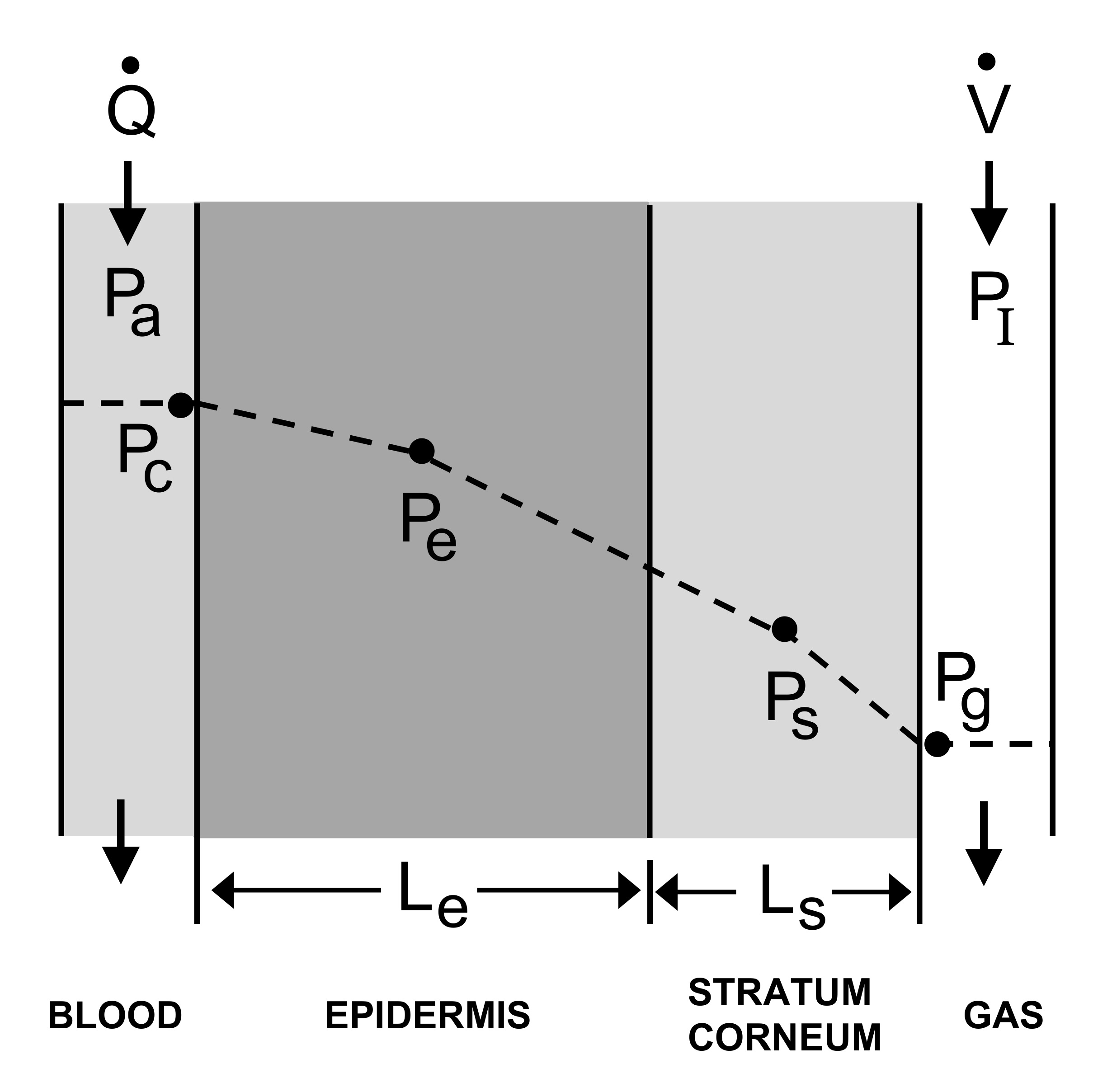
The kinetics of ethanol transport from the blood to the skin surface are
incompletely understood. We present a mathematical model to predict the
transient exchange of ethanol across the skin while it is being absorbed
from the gut and eliminated from the body. The model simulates the
behavior of a commercial device that is used to estimate the blood alcohol
concentration (BAC). During the elimination phase, the stratum corneum
of the skin has a higher ethanol concentration than the blood. We studied
the effect of varying the maximum BAC and the absorption rate from the
gut on the relationship between BAC and equivalent concentration in the
gas phase above the skin. The results showed that the ethanol concentration
in the gas compartment always took longer to reach its maximum,
had a lower maximum, and had a slower apparent elimination rate than
the BAC. These effects increased as the maximum BAC increased. Our
model’s predictions are consistent with experimental data from the
literature. We performed a sensitivity analysis (using Latin hypercube
sampling) to identify and rank the importance of parameters. The analysis
showed that outputs were sensitive to solubility and diffusivity within the
stratum corneum, to stratum corneum thickness, and to the volume of gas
in the sampling chamber above the skin. We conclude that ethanol
transport through the skin is primarily governed by the washin and
washout of ethanol through the stratum corneum. The dynamics can be
highly variable from subject to subject because of variability in the
physical properties of the stratum corneum.
Figure
Equations
The equations for this model may be viewed by running the JSim model and clicking on the Source tab at the bottom left of JSim's Run Time graphical user interface. Equations can also be viewed by downloading the MML code text file. The equations are written in JSim's Mathematical Modeling Language (MML). See the Introduction to MML and the MML Reference Manual. Additional documentation for MML can be found by using the search option at the Physiome home page.
- Download JSim model MML code (text):
- Download translated SBML version of model (if available):
We welcome comments and feedback for this model. Please use the button below to send comments:
1. Hlastala MP, and Anderson JC. Alcohol breath test: gas exchange issues. J Appl
Physiol 121: 367-375, 2016.
2. Dougherty DM, Hill-Kapturczak N, Liang Y, Karns TE, Cates SE, Lake SL,
Mullen J, and Roache JD. Use of continuous transdermal alcohol monitoring
during a contingency management procedure to reduce excessive alcohol use.
Drug and alcohol dependence 142: 301-306, 2014.
3. Marques PR, and McKnight AS. Evaluating Transdermal Alcohol Measuring
Devices National Highway Traffic Safety Administration, 2007.
4. Wang Y, Fridberg DJ, Leeman RF, Cook RL, and Porges EC. Wrist-Worn
Alcohol Biosensors: Strengths, Limitations, and Future Directions. Alcohol
(Fayetteville, NY) 81: 83-92, 2019.
5. Anderson JC, and Hlastala MP. The kinetics of transdermal ethanol exchange. J
Appl Physiol 100: 649-655, 2006.
6. Karns-Wright TE, Roache JD, Hill-Kapturczak N, Liang Y, Mullen J, and
Dougherty DM. Time Delays in Transdermal Alcohol Concentrations Relative to
Breath Alcohol Concentrations. Alcohol and alcoholism (Oxford, Oxfordshire) 52:
35-41, 2017.
7. Marques PR, and McKnight AS. Field and laboratory alcohol detection with 2
types of transdermal devices. Alcohol Clin Exp Res 33: 703-711, 2009.
8. Dumett M, Rosen G, Sabat J, Shaman A, Tempelman L, Wang C, and Swift R.
Deconvolving an Estimate of Breath Measured Blood Alcohol Concentration from
Biosensor Collected Transdermal Ethanol Data. Applied mathematics and
computation 196: 724-743, 2008.
9. Rosen IG, Luczak SE, and Weiss J. Blind Deconvolution for Distributed
Parameter Systems with Unbounded Input and Output and Determining Blood
Alcohol Concentration from Transdermal Biosensor Data. Applied mathematics
and computation 231: 357-376, 2014.
10. Webster G, and Gabler H. Feasibility of Transdermal Ethanol Sensing for the
Detection of Intoxicated Drivers. Annual proceedings/Association for the
Advancement of Automotive Medicine 51: 449-464, 2007.
11. Webster GD, and Gabler HC. Modeling of transdermal transport of alcohol: effect
of body mass and gender. Biomedical sciences instrumentation 44: 361-366, 2008.
12. Anderson JC, Babb AL, and Hlastala MP. Modeling soluble gas exchange in the
airways and alveoli. Ann Biomed Eng 31: 1402-1422, 2003.
13. Carlson BE, Anderson JC, Raymond GM, Dash RK, and Bassingthwaighte
JB. Modeling oxygen and carbon dioxide transport and exchange using a closed
loop circulatory system. Adv Exp Med Biol 614: 353-360., 2008.
14. Bird RB, Stewart WE, and Lightfoot EN. Transport phenomena. New York: John
Wiley & Sons, 1960.
15. Bui TD, Dabdub D, and George SC. Modeling bronchial circulation with
application to soluble gas exchange: description and sensitivity analysis. Journal
of Applied Physiology 84: 2070-2088, 1998.
16. Butterworth E, Jardine BE, Raymond GM, Neal ML, and Bassingthwaighte
JB. JSim, an open-source modeling system for data analysis. F1000Research 2:
288, 2013.
17. Widmark EMP. Principles and Applications of Medicolegal Alcohol Determination
(Die theoretischen Grundlagen und die praktische Verwendbarkeit der
gerichtlichmedizinischen Alkoholbestimmung, Berlin: 1932). Davis, Calif.:
Biomedical Pubs., 1981.
18. Blower SM, and Dowlatabadi H. Sensitivity and uncertainty analysis of complex
models of disease transmission: an HIV model, as an example. International
Statistical Review 62: 229-243, 1994.
19. Brown DJ. The pharmacokinetics of alcohol excretion in human perspiration.
Methods Find Exp Clin Pharmacol 7: 539-544, 1985.
20. Swift R. Transdermal alcohol measurement for estimation of blood alcohol
concentration. Alcohol Clin Exp Res 24: 422-423, 2000.
21. Swift RM, Martin CS, Swette L, LaConti A, and Kackley N. Studies on a
wearable, electronic, transdermal alcohol sensor. Alcohol Clin Exp Res 16: 721-
725, 1992.
22. Lawson B, Aguir K, Fiorido T, Martini-Laithier V, Bouchakour R, Burtey S,
Reynard-Carette C, and Bendahan M. Skin alcohol perspiration measurements
using MOX sensors. Sensors and Actuators B: Chemical 280: 306-312, 2019.
23. Blank IH, Moloney J, 3rd, Emslie AG, Simon I, and Apt C. The diffusion of water
across the stratum corneum as a function of its water content. The Journal of
investigative dermatology 82: 188-194, 1984.
24. Wu MS, Yee DJ, and Sullivan ME. Effect of a skin moisturizer on the water
distribution in human stratum corneum. The Journal of investigative dermatology
81: 446-448, 1983.
25. Scheuplein RJ, and Blank IH. Permeability of the skin. Physiol Rev 51: 702-747,
1971.
26. Scheuplein RJ, and Blank IH. Mechanism of percutaneous absorption. IV.
Penetration of nonelectrolytes (alcohols) from aqueous solutions and from pure
liquids. The Journal of investigative dermatology 60: 286-296, 1973.
27. Dancik Y, Miller MA, Jaworska J, and Kasting GB. Design and performance of
a spreadsheet-based model for estimating bioavailability of chemicals from dermal
exposure. Advanced drug delivery reviews 65: 221-236, 2013.
28. Gajjar RM, and Kasting GB. Absorption of ethanol, acetone, benzene and 1,2-
dichloroethane through human skin in vitro: a test of diffusion model predictions.
Toxicology and applied pharmacology 281: 109-117, 2014.
29. Li B, Downen RS, Dong Q, Tran N, LeSaux M, Meltzer AC, and Li Z. A Discreet
Wearable IoT Sensor for Continuous Transdermal Alcohol Monitoring - Challenges
and Opportunities. IEEE sensors journal 21: 5322-5330, 2021.
30. Jalal AH, Umasankar Y, Gonzalez PJ, Alfonso A, and Bhansali S. Multimodal
technique to eliminate humidity interference for specific detection of ethanol.
Biosensors & bioelectronics 87: 522-530, 2017.
31. Jalal AH, Umasankar Y, Pretto EA, and Bhansali S. A wearable micro-fuel cell
sensor for the determination of blood alcohol content (BAC): a multivariate
regression model approach. ISSS Journal of Micro and Smart Systems 9: 131-
142, 2020.
32. Dai Z, Rosen IG, Wang C, Barnett N, and Luczak SE. Using drinking data and
pharmacokinetic modeling to calibrate transport model and blind deconvolution
based data analysis software for transdermal alcohol biosensors. Mathematical
biosciences and engineering : MBE 13: 911-934, 2016.
33. Luczak SE, and Rosen IG. Estimating BrAC from transdermal alcohol
concentration data using the BrAC estimator software program. Alcohol Clin Exp
Res 38: 2243-2252, 2014.
34. Anderson JC, and Hlastala MP. The alcohol breath test in practice: effects of
exhaled volume. J Appl Physiol 126: 1630-1635, 2019.
35. Hlastala MP, and Anderson JC. The impact of breathing pattern and lung size on
the alcohol breath test. Ann Biomed Eng 35: 264-272, 2007.
36. Hill-Kapturczak N, Roache JD, Liang Y, Karns TE, Cates SE, and Dougherty
DM. Accounting for sex-related differences in the estimation of breath alcohol
concentrations using transdermal alcohol monitoring. Psychopharmacology 232:
115-123, 2015.
37. Giacomoni PU, Mammone T, and Teri M. Gender-linked differences in human
skin. Journal of dermatological science 55: 144-149, 2009.
38. Luebberding S, Krueger N, and Kerscher M. Skin physiology in men and women:
in vivo evaluation of 300 people including TEWL, SC hydration, sebum content and skin
surface pH. International journal of cosmetic science 35: 477-483, 2013
Please cite https://www.imagwiki.nibib.nih.gov/physiome in any publication for which this software is used.
Model development and archiving support at https://www.imagwiki.nibib.nih.gov/physiome provided by the following grants: NIH U01HL122199 Analyzing the Cardiac Power Grid, 09/15/2015 - 05/31/2020, NIH/NIBIB BE08407 Software Integration, JSim and SBW 6/1/09-5/31/13; NIH/NHLBI T15 HL88516-01 Modeling for Heart, Lung and Blood: From Cell to Organ, 4/1/07-3/31/11; NSF BES-0506477 Adaptive Multi-Scale Model Simulation, 8/15/05-7/31/08; NIH/NHLBI R01 HL073598 Core 3: 3D Imaging and Computer Modeling of the Respiratory Tract, 9/1/04-8/31/09; as well as prior support from NIH/NCRR P41 RR01243 Simulation Resource in Circulatory Mass Transport and Exchange, 12/1/1980-11/30/01 and NIH/NIBIB R01 EB001973 JSim: A Simulation Analysis Platform, 3/1/02-2/28/07.